Hot on the Scent
Incompatible MatingThe best smell in the world is that man that you love. - Jennifer Aniston
To the ancient Greeks, the Chimæra was a female monster. It had the head of a lion, the body of a goat and the tail of a serpent. And it breathed fire. Fortunately it was unique. Modern biology, too, recognises chimæras. Like the one that terrorised ancient Lycia, they are mixed-up creatures. They are composed of cells which, while not from different species, have more than one genetic pedigree. They are also generally female. But far from being unique, they are ubiquitous. For, to biologists, every pregnant mammal is a chimæra. This creates an awkwardness for a pregnant creature's immune system. This system is designed to recognise foreign tissues (which usually belong to parasites), and destroy them. A fœtus, however, is also foreign tissue, because half of its genes (and therefore lots of the proteins of which it is made) are paternal. And, though a few mothers might regard their fœtuses as parasites, natural selection cannot afford to. So, by a mechanism that is not yet well understood, fœtuses are exempted from the attentions of the maternal immune system. This exemption appears to carry a price: the immune system that is so gentle with the child often seems to turn on the mother. As a consequence, women are more vulnerable than men to auto-immune diseases - those where the immune system becomes confused and starts attacking the body it is meant to defend. The Chimæra's BreathOne such disease is scleroderma, a painful condition in which the skin thickens and hardens like the shell of a turtle. The fact that scleroderma is 10 times more common in women than in men is usually attributed to œstrogen, the principal female sex hormone. But Lee Nelson, an immunologist at the Fred Hutchinson Cancer Research Centre in Seattle, Washington, thinks that blaming œstrogen leaves too much unexplained. She suspects that, at least sometimes, scleroderma could be a consequence of a woman's exposure to her mate's genes during pregnancy. And she has noticed a similarity between scleroderma and an illness sometimes suffered by those who have undergone bone-marrow transplants: graft-versus-host disease. Bone marrow acts, among other things, as a manufacturing plant for the cells of the immune system. Replacing it is often part of treatment for leukæmia. But the donated marrow must be a reasonable genetic match for the host. In particular, the genes for the "major histocompatibility complex" (MHC) must match well, because MHC genes carry the plans for a group of proteins (known as MHC class I and class II molecules) that sit on the surfaces of cells and are recognised by the immune system. If the graft cells cannot recognise that the host MHC proteins are like their own, they will regard the host as alien and attack his cells. Dr Nelson reckons that scleroderma might be caused by a variation on this theme, with fœtal cells attacking those of the mother. The weakness of this hypothesis is that women do not usually get scleroderma during a pregnancy; sufferers are generally between 35 and 45, an age by which most women have had their children. Dr Nelson's idea would therefore be plausible only if women remained chimæric after giving birth - in other words, if fœtal cells remained inside them. Diana Bianchi, at Tufts University's New England Medical Center in Boston, believes she has evidence of this happening. She and her team have discovered cells bearing Y-chromosomes, which are normally found only in male cells, hiding in the bloodstreams of a number of their female subjects. Perhaps, she reckons, these Y-carrying cells are left over from earlier pregnancies - an idea consistent with the fact that they have been found only in women who have had sons. Nor were these any old fœtal cells. The cells Dr Bianchi detected were "progenitor cells", which means that they could one day become active members of an immune system. No one knows whether they do actually become active. But if they do, they might start attacking the cells of the mother. Since a fœtus acquires half of its genes from its mother, at least half of the MHC proteins will be the same in mother and child. Whether the other half are also similar depends on who the father is. But if it so happened that the father's contribution were similar to the mother's, a combination of MHC proteins could arise that allowed the mother's immune system to overlook a few rogue fœtal cells in her body. These cells might then see the mother as foreign and launch an attack on her. If Dr Nelson is right, scleroderma ought to be more likely to occur in women whose mates share MHC genes with them. Her preliminary results suggest that this is, indeed, the case. Hot on the ScentAs it happens, evolutionary biologists have long thought it a bad idea to choose a mate with MHC molecules similar to your own. The reason is that different MHC molecules are good at recognising different parasitic invaders. So the larger the variety of MHC molecules you possess, the more likely you are to be able to resist a wide range of infectious diseases. To promote the survival of her offspring, a female should therefore prefer - other things being equal - to mate with a male whose MHC complex is different from her own. That female mice do indeed show such preferences has already been established. Research by Claus Wedekind and his colleagues at the University of Bern, in Switzerland, now suggests that female people behave the same way. MHC proteins affect the odour of mammals. Human nostrils can distinguish between strains of mice whose only genetic differences lie in their MHCS. Mice and dogs seem to be able to tell the difference both with respect to members of their own species and with respect to people. So Dr Wedekind and his colleagues decided to test whether smell can attract particular women to particular men - and whether that has anything to do with the MHC. In an experiment last year the team gave T-shirts to 44 male students at the University of Bern, asking them to wear the shirts for two nights in a row, and to avoid using deodorants or scented soaps until the experiment was over. Then, 49 female students were invited to sniff 6 T-shirts each. The women were presented with 3 T-shirts worn by men with different MHC genes from their own, and 3 worn by men with similar MHC genes. The results were striking. As predicted, most women preferred the smells of men who had a different set of MHC genes. But 18 of the women - those who were taking contraceptive pills at the time - preferred the smell of men with MHC genes like their own. If this result is confirmed, it suggests that widespread pill use could be having a subtle effect on how women select their mates - and perhaps on whether they will suffer from auto-immune diseases. Not all auto-immune diseases are likely to be caused by the mechanism Dr Nelson proposes. Some, such as rheumatoid arthritis, seem to go into abeyance during pregnancy. But even these are more common among women than men. And the MHC does seem to play a role. In previous work Dr Nelson has found that pregnant women whose arthritis had gone into remission tended to have mated with partners whose MHCs were different from theirs. It used to be thought that auto-immune diseases became less virulent during pregnancy because a woman's immune system is "turned down" to protect the fœtus. But this explanation is now out of favour. Why if it were true, are pregnant women not prey to the risk of infection experienced by organ-transplant patients whose immune systems are suppressed by drugs? Miriam Richards, a biologist at Brock University, in Ontario, has another explanation for what is happening. She links that a fœtus might induce permanent changes in the cells of a mother's immune system. Last year, Anna Tafuri and her colleagues at Heidelberg University, in Germany, showed that during pregnancy a mother's immune system changes so that it temporarily recognises - and tolerates - the father's genes. Dr Richards thinks that these changes may sometimes last forever. Exactly why such changes might prevent or moderate auto-immune diseases remains unclear. But it seems that from every point of view, choosing a mate who smells sweet is a wise thing to do. Source: The Economist 21 September 1996 Illustration: The Chimera of Amiens 1910 drypoint by Sir David Young Cameron
Compatible Mating (If You Pick the Right Mate...)Cells from Babies Help Heal their Mothersby Alison Motluk Pregnancy certainly has its downside, but it may have an unexpected upside as well: cells from the baby may help heal wounds in the mother, even long after it has been born. It has been known for about a decade that cells from a human fœtus can remain in its mother’s blood and bone marrow for many years. But what do they do? Diana Bianchi at the Tufts-New England Medical Center in Boston and her colleagues recently showed that these fœtal cells can transform themselves into specialised cells in the thyroid, intestine, cervix and gall bladder. Now her team has shown that, in mice at least, these fœtal cells also help heal skin wounds in the mother, both during and after pregnancy. To make it easy to spot the fœtal cells, the researchers mated normal females with males whose cells had been genetically engineered to glow when the gene for VEGFR2, a blood vessel growth factor, is switched on. The fœtal cells would thus glow too if involved in blood vessel formation in growing or healing tissues. In the pregnant mice, the glow initially came only from the placenta, as expected. But when small cuts were made in the skin of the mice, glowing cells appeared at the site of the wound, reaching a peak after five days, Bianchi told a meeting of the American Society of Human Genetics in Toronto last week. What remains unclear is the relative contribution of fœtal cells to the healing process compared with maternal cells, something the team hopes to look at. Three weeks after the pups had been born, the fœtal cells were still helping to heal wounds in the mothers. "I’d like to think you get some payback for pregnancy," says Bianchi. "The fœtus has a vested interest in keeping the mother healthy." She notes that the condition of women with autoimmune disorders such as rheumatoid arthritis or multiple sclerosis often improves while they are pregnant. But it is not all good news: there is also some evidence that fœtal cells that linger in the mother can sometimes trigger autoimmune disorders (see article at the top of this page). Source: newscientist.com 8 November 2004
Baby Comes with Brain Repair Kit for Mumby Andy Coghlan Everyone knows that kids get their brains, or lack of them, from their parents. But it now seems that the reverse is also true. Stray stem cells from a growing fœtus can colonise the brains of mothers during pregnancy, at least in mice. If the finding is repeated in humans, the medical implications could be profound. Initial results suggest that the fœtal cells are summoned to repair damage to the mother's brain. If this is confirmed, it could open up new, safer avenues of treatment for brain damage caused by strokes and Alzheimer's disease, for example. This is a long way off, but there are good reasons for thinking that fœtal stem cells could one day act as a bespoke brain repair kit. It is already well known that during pregnancy a small number of fœtal stem cells stray across the placenta and into the mother's bloodstream, a phenomenon called microchimerism. They can survive for decades in tissues such as skin, liver and spleen, where they have been shown to repair damage. Nature's ploy to "treat mother" makes evolutionary sense too, because the fœtus has a better chance of survival if the mother is fit and healthy both during and after pregnancy. But nobody has seen this effect in brain cells. "This is the first study to show conclusively that fœtal cells cross the blood-brain barrier," says Diana Bianchi, a world authority on microchimerism at Tufts University School of Medicine in Boston, Massachusetts. A team led by Gavin Dawe of the National University of Singapore and Xiao Zhi-Cheng of Singapore's Institute of Molecular and Cell Biology showed that once the stowaways enter mouse brains, they mature into different cell types. These include cells resembling neurons, which transmit electrical impulses; astrocytes, which support neurons; and oligodendrocytes, which ensheath and protect nerve cells. "They can become almost all major cell types found in the brain," Dawe says. The researchers have not yet demonstrated whether the cells are functional, however. "We need to know, for example, whether fœtal cells expressing characteristics of neuronal cells can actually fire action potentials and synapse with native cells in the mother's brain," he adds. To make fœtal stowaways easy to spot in samples from the mother's brain, Dawe and Xiao mated normal female mice with male mice genetically engineered so that their cells contained a fluorescing protein derived from jellyfish, making the cells glow bright green. This revealed that the fœtal cells did not spread evenly. When the researchers induced stroke-like injuries to the brains of some of the mother mice, the fœtal cells became 6 times more concentrated at the damaged areas, suggesting they may be involved in repair (Stem Cells, DOI: 10.1634/stemcells.2004-0169). Dawe says it is not yet clear how they are summoned to the sites of injury, but he suspects they are drawn there by "SOS-like" signalling factors from damaged tissue. The team is also trying to identify surface molecules unique to the brain-bound fœtal cells, and hopes to isolate human counterparts from umbilical blood or bone marrow. This would be vital for medical applications, as a large number of cells might be needed to have any medical effect. "It would be important to enrich for ones that can cross the blood-brain barrier," Dawe says. A big potential advantage of using fœtal cells as a treatment is that they could simply be injected into the bloodstream and left to find their own way into the brain. This would make it possible to treat conditions with diffuse injury, such as Alzheimer's disease. The only existing way of getting cells into the brain to treat injured or defective areas is to inject them directly through the skull into the area where they are required. Parkinson's disease, for example, has been treated by injecting cells that make the neurotransmitter dopamine into the region of the brain that fails to make the substance in Parkinson's patients. Some researchers have shown, however, that injected fœtal cells are capable of migrating across the brain to sites of damage. Dawe and Xiao warn that it could take anything from 5 to 20 years to develop treatments, not least because in some cases, fœtal cells have been shown to aggravate immunological disease. "It's important we know it's safe and of benefit before we try it in patients," Dawe cautions. One key step will be to establish beyond doubt that the effect seen in mice happens in humans too. Dawe says this can be done by looking for cells containing a Y chromosome in post-mortem brain tissue from mothers of boys. "We've already started work on acquiring tissue to answer this question," he says. Bianchi says that most research on microchimerism in mice has later been borne out in humans. "In every aspect, the trend has been the same," she says. But even if the phenomenon does occur in people, there are many hurdles to be cleared on the way to developing treatments. "It's unclear how long the newly arrived cells will live, and how well they would integrate into the specialised functional networks of the brain," says Jakub Tolar, a specialist in microchimerism at the University of Minnesota in Minneapolis. "Predictions of clinical use must come with caution and reflection." Weblinks
Source: newscientist.com 20 August 2005
Baby to Brain: Therapy Clues from Fœtal Cells that Enter Mom's Brainby Charles Q Choi Mothers could literally always have their kids on their minds. Researchers find that in mice, cells from fœtuses can migrate into a mother's brain and apparently develop into nervous system cells. The discovery comes from Gavin S Dawe of the National University of Singapore and Zhi-Cheng Xiao of Singapore General Hospital, along with their colleagues from China and Japan. They were looking to design therapies for stroke or diseases such as Alzheimer's. Scientists have known for years that fœtal cells can enter a mother's blood; in humans, they may remain there at least 27 years after birth. Like stem cells, they can become many other kinds of cells and in theory might help repair damaged organs. The neurobiologists bred normal female mice with males genetically modified to uniformly express a green fluorescent protein. They found green fœtal cells in the mothers' brains. "In some regions of some mothers' brains, there are as many as one in 1,000 to sometimes even 10 in 1,000 cells of fœtal origin," Xiao reports. The fœtal cells transformed into what seem like neurons, astrocytes (which help to feed neurons), oligodendrocytes (which insulate neurons) and macrophages (which ingest germs and damaged cells). Moreover, after the scientists chemically injured the mouse brains, nearly 6 times as many fœtal cells made their way to damaged areas than elsewhere, suggesting the cells could be responding to molecular distress signals released by the brain. Just how the fœtal cells make it through the capillaries separating the brain from the blood system is not known - the cells of the vessels are densely packed, preventing most compounds from crossing the barrier. The researchers speculate that biomolecules such as proteins or sugars adorning fœtal cell surfaces interact with the blood-brain barrier and allow the cells to wriggle past. The team feels confident that fœtal cells can also pass to the brains of males and nonpregnant females, given little evidence of major differences between their blood-brain barriers and those of pregnant females, Dawe says. The scientists hope next to show that the fœtal cells become functional neurons. The finding, published online 10 August 2005 by Stem Cells, gives fresh hope in treating brain disorders. Because of the blood-brain barrier, transplant therapies for the brain normally evoke thoughts of drilling into the skull. Identifying the molecules typical of fœtal cells that enter the brain and become nervous system cells could help find similar cells from sources other than fœtuses, such as umbilical cord blood. Such research could lead to noninvasive cell transplants for the brain requiring only intravenous injections. Any cells used for therapies would be matched to patients as closely as possible to avoid triggering immune disease. It remains uncertain whether injected cells meant for the brain could end up grafting somewhere else, "but we don't know yet if that happening would even be a problem," Dawe says. The investigators are also now looking to see if the passage of fœtal cells to the brain occurs in humans as readily as it does in mice. They plan on looking at postmortem brain tissue from mothers of boys. Signs of a Y chromosome would confirm the effect in humans. It would also, Xiao points out, raise the issue of "whether there are any behavioural or psychological implications." Source: sciam.com 31 October 2005
Fœtal cell "Transplant" Could Be a Hidden Link between Childbirth and Reduced Risk of Breast CancerPhiladelphia – Some benefits of motherhood are intangible, but one has been validated through biostatistical research: women who bear children have a reduced risk of developing breast cancer. In Seattle, Washington, researchers at the University of Washington and Fred Hutchinson Cancer Research Center believe they have identified a source of this protective effect: fœtal cells “transplanted” to the mother before birth. Their findings are presented in the 1 October issue of Cancer Research, a journal of the American Association for Cancer Research. The ability of cells from a growing fœtus to take up long-term residence within its mother is a phenomenon called fœtal microchimerism. According to the researchers, while fœtal microchimerism has been implicated as a mechanism of autoimmune disease, it may also benefit mothers by putting the immune system on alert for malignant cells to destroy. To test the idea, the researchers recruited 82 women, 35 of whom had been diagnosed with breast cancer. Approximately two-thirds of the women studied have had children, and more than half of the participants had given birth to at least one son. The researchers took blood samples from each participant and searched them for male DNA, as they reasoned it is a relatively definitive matter to detect the male Y chromosome amid the mother’s native – and obviously female – cells within a blood sample. Among the women with breast cancer, only five had male DNA in their bloodstream. Three of the five previously gave birth to sons, one had had an abortion and the other had never been knowingly pregnant. In total, about 14% of all women in the breast cancer group had male DNA in their bloodstream compared to 43% of women in the non-breast cancer group. "Our research found that these persisting fœtal cells may be giving a woman an edge against developing breast cancer,” said lead author Vijayakrishna K Gadi, MD, PhD, assistant professor at the University of Washington and research associate at the Fred Hutchinson Cancer Research Center. “This experiment of nature is all the more fascinating because for years doctors treated a number of different cancers by transplanting cells from one person to another." According to Dr Gadi, these findings could provide a starting point for future research on the role of fœtal microchimerism in the prevention of cancer. In addition, there are other reasons for male DNA to be in a woman’s peripheral blood, such as miscarriage and abortion – or possibly even blood transfusion or a male twin that was reabsorbed into the womb at an early stage of the pregnancy. in prior studies the prevalence of T, B, natural-killer (NK) and antigen-presenting cells of fœtal origin in healthy women ranged from 30% to 70%, depending on the cell type. Sources: eurekalert.org (1) and eurekalert.org (2) American Association for Cancer Research and the Fred Hutchinson Cancer Research Center 2 October 2007
However, the news is not always good... Mother's RuinReverse inheritance happens during pregnancy and is caused by cells from the fœtus making their way into the mother's bloodstream and staying there for years... Scleroderma, which hardens the skin and then goes on to immobilise many of the body's internal organs, looks very different from multiple sclerosis, which cripples its victims by stripping away the protective sheaths of their nerve cells. Systemic lupus erythematosus, which can fatally damage the kidneys, looks different again. Yet they have something in common. They and more than 70 other diseases - including such familiar ailments as psoriasis and rheumatoid arthritis - are all the result of the immune system mistaking one or another of the proteins that the body makes as being "foreign" rather than "self". This misidentification means that the immune system attacks cells containing that protein as if they were invading bacteria or viruses. Many researchers view such autoimmune disorders as members of a family, with the same underlying mechanism and varying only in the details of what has gone wrong and where. According to the researchers who addressed the AAAS session on autoimmune diseases, that familial relationship helps to explain why these illnesses do not obey the usual rules of inheritance. Noel Rose, an immunologist at Johns Hopkins University in Baltimore, pointed out that if these diseases were entirely genetic then if one identical twin had such a disease the other might be expected to come down with it, too. In fact, no autoimmune disease has more than a 50% chance of appearing in one twin if the other is affected, and with some diseases, such as early-onset or "type 1" diabetes, that figure is only about 5%. In Dr Rose's view, what is often being inherited is not a genetic predisposition to a particular autoimmune disease, but rather a generalised predisposition to the whole class of them. Which disorder actually develops is more or less accidental. This generalised predisposition has been demonstrated by another of the session's speakers, Denise Faustman, of the Massachusetts General Hospital in Boston. She has been studying a strain of laboratory mice which has been bred so that its members are genetically identical. These mice tend to develop a form of type 1 diabetes that closely mimics its human counterpart. Despite their genetic identity, however, about 20% of them are healthy. This led Dr Faustman to wonder what would happen if she mated healthy males and females. The offspring of these unions did not become diabetic either, but some of the females in the resulting litters developed rheumatoid arthritis when they reached reproductive age. This suggests that the same set of "autoimmunity" genes can result in different outcomes. Such findings also highlight a second curious feature of autoimmune diseases - that in all species studied so far, they affect females more than males. Women are three times as likely to be afflicted as men. The reason seems to be that besides genetic inheritance, autoimmunity is subject to a second, and very odd, form of "heredity": you can get it from your children. This reverse inheritance happens during pregnancy and is caused by cells from the fœtus making their way into the mother's bloodstream and staying there for years, a condition known as "microchimærism". J Lee Nelson, at the Fred Hutchinson Cancer Centre in Seattle, has found that women with scleroderma have at least 10 times more fœtal cells in their blood after the birth of a baby than mothers who are free of the dreadful disease. Dr Nelson speculates that such microchimærism is disrupting normal interactions in the mother's immune system. This interference might cause scleroderma, which it resembles, versus host disease, another nasty immune reaction caused by a mixing of cells which occurs when a mismatched tissue transplant attacks the body of its new owner. Much more work needs to be done to understand exactly how fœtal cells might wreak such havoc in the mother. Sharper than a serpent's tooth, indeed. Source: The Economist 24 February 2001
I wonder if some forms of alopecia areata (hair loss) in women are due to microchimærism. I read this on an alopecia-sufferer's website (italics are mine): "Two to three months after a severe illness (especially one with bouts of fever) or childbirth, scalp hair may be shed in abundance." Our bodies house amazing chemical processes, some of which we can modify through what we ingest, inhale or (in the case of falling in love) infer. See also:
On the Other Hand: Womb Environment "Makes Men Gay"A man's sexual orientation may be determined by conditions in the womb, according to a study. Previous research had revealed the more older brothers a boy has, the more likely he is to be gay, but the reason for this phenomenon was unknown. But a Canadian study has shown that the effect is most likely due to biological rather than social factors. The research is published in the journal of the Proceedings of the National Academy of Sciences. Professor Anthony Bogaert from Brock University in Ontario, Canada, studied 944 heterosexual and homosexual men with either "biological" brothers, in this case those who share the same mother, or "non-biological" brothers, that is, adopted, step or half siblings. He found the link between the number of older brothers and homosexuality only existed when the siblings shared the same mother. The amount of time the individual spent being raised with older brothers did not affect their sexual orientation. Writing in the journal, Professor Bogaert said: "If rearing or social factors associated with older male siblings underlies the fraternal birth-order effect [the link between the number of older brothers and male homosexuality], then the number of non-biological older brothers should predict men's sexual orientation, but they do not. "These results support a prenatal origin to sexual orientation development in men." He suggests the effect is probably the result of a "maternal memory" in the womb for male births. A woman's body may see a male foetus as "foreign", he says, prompting an immune reaction which may grow progressively stronger with each male child. The antibodies created may affect the developing male brain. In an accompanying article, scientists from Michigan State University said: "These data strengthen the notion that the common denominator between biological brothers, the mother, provides a prenatal environment that fosters homosexuality in her younger sons. But the question of mechanism remains." Andy Forrest, a spokesman for gay rights group Stonewall, commenting on this and other studies, said: "Increasingly, credible evidence appears to indicate that being gay is genetically determined rather than being a so-called lifestyle choice. It adds further weight to the argument that lesbian and gay people should be treated equally in society and not discriminated against for something that's just as inherent as skin colour." Source: news.bbc.co.uk 27 June 2006
This Makes ScentsCor, You Don't Half SmellDid you dab on a little cologne this morning? Using scent to make yourself more attractive is nothing new. People have been dousing themselves with fragrances since at least the time of the ancient Egyptians. But, perhaps surprisingly, nobody really knows why. The general assumption is that perfume is a form of olfactory camouflage for foul body odour. But research by Manfred Milinski of the Max Planck Institute in Ploen, Germany, and Claus Wedekind of the University of Edinburgh, to be published soon in Behavioral Ecology, suggests the reason could be the opposite: to underscore a person's existing smell. Dr Milinski and Dr Wedekind asked 137 students (of both sexes) at the University of Bern to sniff a range of 36 odours. These included such familiar fragrances as rose and geranium - but also more exotic ones such as ambergris, a substance regurgitated from the intestines of sperm whales, and musk, which is scooped from an Asian deer's abdominal gland, both of which are prized perfume ingredients. The students were asked to decide if a particular fragrance was suitable for themselves, ranking it from "pleasant" to "unpleasant". Then they were asked to repeat the experiment, this time asking whether each smell would be appealing on a mate. Previous work has shown that a cluster of genes called the major histocompatibility complex, or MHC, helps to determine body odour. The MHC is part of the immune system, and varies from individual to individual, although relatives have more similar MHCs than do the unrelated. In mice, individuals are known to use this information when they are choosing mates - presumably to avoid inbreeding. And in the past Dr Wedekind has found evidence suggesting that this may be true of people, too. He and Dr Milinski therefore took blood samples from their volunteers, in order to analyse their MHC genes. They reckoned that, if people were choosing perfumes to augment their own natural smells, then those with similar MHC genes would tend to prefer the same scents. And that is precisely what they found. The results were strongest for those who had the genes known as HLA-A1 and HLA-A2 in their complexes. People with HLA-A1, for example, tended to dislike ambergris and musk, while those with HLA-A2 rather liked them. There was no association, however, between a person's MHC and the kind of scent they preferred on a mate - a reasonable observation, according to Dr Milinski, since anything other than "self" could smell appealing on a partner. These results are quite in keeping with perfume history, according to Dr Milinski. In medieval times, professional perfumers would concoct personal scents for their clients from 6 to 8 special ingredients. A daughter would inherit a few of those ingredients from her mother. He also points out that, despite the fact that perfume companies come out with new products every year, the ingredients remain largely unchanged - and still include many substances identified in Biblical perfume recipes. That which we call a rose, by any other name might smell as sweet. But only if the right person is wearing it. Source: The Economist 27 January 2001
How the Contraceptive Pill Could Stop Women Sniffing out Their Perfect Partner through His Sweatby Fiona Macrae They say that opposites attract. But it seems the Pill may be preventing women sniffing out men who are opposite enough. Women are said to have an inbuilt ability to pick up the scent of a partner who differs genetically. Falling for this type of man helps ensure that the couple's children will have broad immunity against disease, so the theory goes. But researchers found that the Pill disrupts a woman's power to recognise the aroma of a suitable partner. Saddled with the wrong man - someone who in scientific terms has similar genes - she may find it hard to become pregnant and any children she does have may have a lower resistance to infection. What is more, when she stops taking the Pill and her sense of smell returns to normal, she's more likely to fall out of love, the Liverpool and Newcastle universities research suggests. It is thought that women subconsciously use the smell of a man's sweat as a guide to the genetic make-up of his immune system. But this research shows that the Pill sends the rules of attraction into meltdown by making women set their sights on men similar to themselves. To measure its effect, scientists asked a group of men to sleep in T-shirts and steer clear of deodorants and other fragranced products. The T-shirts were frozen until needed, then defrosted and placed in glass jars with "nose holes" in the lids. Almost 100 women then sniffed the shirts and gave their opinions on the "pleasantness" and "desirability" of the odour twice over a 3-month period. Many started taking the Pill during the experiment - and their opinions of the smell of the T-shirts changed, the journal Proceedings of the Royal Society B reports. Researcher Craig Roberts said: "The results showed that the preferences of women who began using the contraceptive Pill shifted towards men with genetically similar odours." Previous studies have shown infertile couples tend to have more similar immune systems than others and that similarity can lead to a roving eye. Dr Roberts said the decision to go on the Pill could have far-reaching consequences. "Although smell is a small thing, it is a fundamental thing. If you really don't like someone's smell, it could lead to the odd argument and you might be more likely to seek out affairs." It is thought the body confuses the hormonal changes caused by the Pill with those of pregnancy. In pregnancy, an altered sense of smell may help a woman bond with relatives who will help her raise her baby. But fertility doctors urged women not to throw away the Pill. Professor Bill Ledger, of Sheffield University, said: "Whilst a relationship is going, I would think the intellectual and emotional feeling you have for that person would surely override what their sweat smells like." Source: dailymail.co.uk 13 August 2008
|
 Animals
Animals Animation
Animation Art of Playing Cards
Art of Playing Cards Drugs
Drugs Education
Education Environment
Environment Flying
Flying History
History Humour
Humour Immigration
Immigration Info/Tech
Info/Tech Intellectual/Entertaining
Intellectual/Entertaining Lifestyles
Lifestyles Men
Men Money/Politics/Law
Money/Politics/Law New Jersey
New Jersey Odds and Oddities
Odds and Oddities Older & Under
Older & Under Photography
Photography Prisons
Prisons Relationships
Relationships Science
Science Social/Cultural
Social/Cultural Terrorism
Terrorism Wellington
Wellington Working
Working Zero Return Investment
Zero Return Investment Smell your mate - for your own health's sake, as well as your
child's
Smell your mate - for your own health's sake, as well as your
child's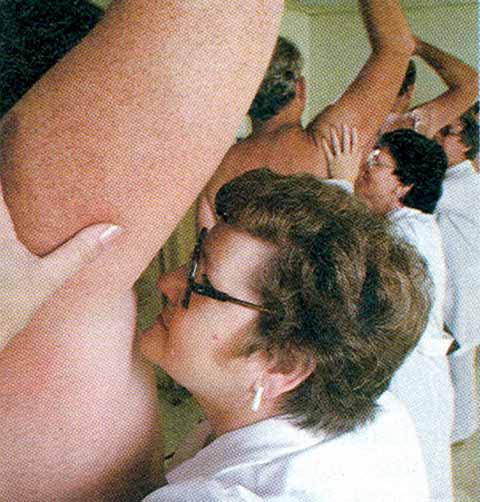 Human Pheromones: The Perfumed Garden
Human Pheromones: The Perfumed Garden